Precise medicine is accurate medicine
Preventative medicine has reached (and keeps reaching) new heights as the human genome is broken down and proclivity to conditions, illnesses, etc. are more predictable. We don’t depend on the information but leveraging it makes medicine a more precise science both in preventing or exacerbating conditions and treating illness and condition. A fascinating article.
More than 40 years ago my mother got a shocking result in her yearly check-up when she was a new immigrant to the US: she had very high cholesterol. The doctors were perplexed, because she was thin and did not have a cholesterol-heavy diet (remember when eggs were bad?). They put her on a very stringent nutritional regime and checked in three months…and the result was the same. They suspected that she had a genetic condition, and prescribed her medication, and the values moved into the normal range. A few years later, in my teens, the same happened to me. And then a few years later, my sister.
Today we know that familial hypercholesterolemia runs in my family. The solution to this is not diet, which has no effect, but medication. The diet was useless, and in fact there is evidence that dietary cholesterol itself has a minimal impact on the levels of cholesterol for the average person. There are certain genetic mutations that change the number of receptors on your cells that mediate the equilibrium level of cholesterol, and some people have an autosomal dominant condition due to a mutation on one of their gene copies that reduces the number of those receptors (roughly, half the receptors mean twice the cholesterol floating around).
And yet in a world where whole-genome sequencing is $200 or less that doesn’t mean there’s a genetic test that can identify if you have a risk for this condition that is very good. I know this because all the genetic tests indicate that my family should have normal serum levels of cholesterol; we clearly carry a variant that hasn’t been studied or included on the panels.
There are tens thousands of Mendelian diseases, those illnesses causes by a single gene mutation. About 10% of Americans have one of these diseases. Meanwhile, illnesses like schizophrenia and type 2 diabatese are highly heritable, though those predispositions are due to mutations at many genetic positions. About 2% of Americans have schizophrenia, while 10% have type 2 diabetes.
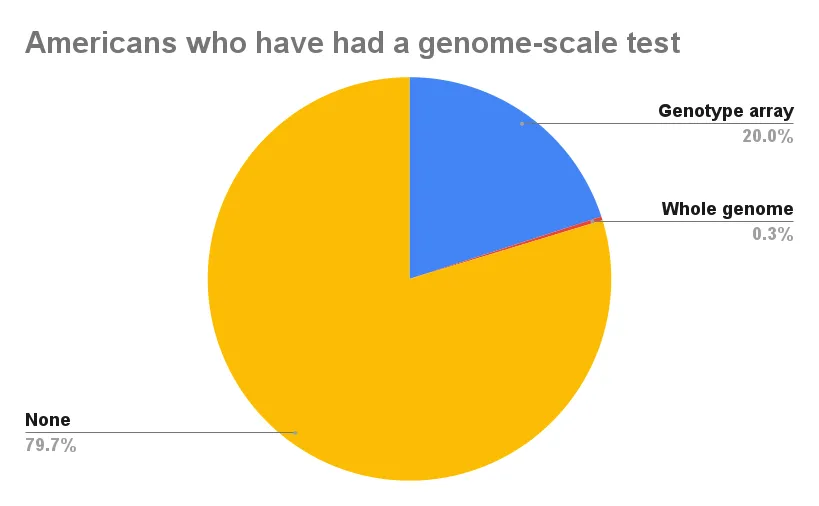
Do you have a predisposition to these disease? Might your children have these diseases? Despite the fact that whole-genome sequencing is the price of a steak dinner for two at Ruth’s Chris, far less than one million out of 330 million Americans have had it done. About 1 in 5 Americans have done some form of direct to consumer genetic testing, whether it be on a single gene, or across 500,000 to 1 million markers (out of 3 billion base-pairs) that is the norm among services like 23andMe, Ancestry and Family Tree DNA.
In 2010 Congress passed Obamacare, which held the promise that all Americans would receive insurance, but also included clauses meant to make healthcare delivery more efficient and information within the system more transparent. On these latter two planks it seems in 2023 we can say that not much has changed. American healthcare is a bureaucratic morass and integration between various parts of the system is still an aspiration, rather than something that has been executed upon.
Your health is the outcome of a variety of factors. The way you live your life (e.g., exercise, nutrition, etc.), your biological characteristics (e.g., your genome, your age, your sex, etc.) and random uncontrolled factors (e.g., whether a coal burning plant is following regulations nearby in terms of emissions). All of these brought together result in morbidity risks, and healthcare professionals can give you recommendations to reduce those risks.
But without all the information one cannot take appropriate precise and directed action. We are all born with genomes (well, without genomes we wouldn’t have been born), and these genomes have hidden within them information that modifies the probabilities of various outcomes in your life. With sequencing and information technology it is potentially accessible to all, and the more information is aggregated into the “data lake” the more insights can be generated. Robustness of prediction and precision of recommendation are conditioned on the variables you have access to. We have the technology, but it hasn’t been brought together under one roof. There are only so many insights you can glean from one million genomes. What’s really required are one billion genomes!
Precision medicine is fundamentally more accurate medicine, because we are all individuals with different risks, often due to our genes. We all need a technological framework that brings together all the different aspects of genomic sequencing and analysis to move through same platform, from raw sequence and health care information, to risk probabilities across a range of traits. That is our goal at GenRAIT, as we aim to make it so that scientists and healthcare professionals don’t need to get a data engineer on the phone. The future is here, even if the past isn’t giving up without a fight. We just need to make it happen.